Measles, herd immunity and the risk of outbreaks
The fine line between epidemics and elimination
Measles vaccines are very effective at stopping measles infections. So effective, in fact, that many countries have managed to stamp out transmission altogether. But there’s a catch: in a susceptible population, measures is very transmissible, which means that we need to vaccinate a very high proportion of the population to bring the reproduction number, R, down below the crucial value of 1.
Unfortunately, as outlined in a recent risk assessment from UKHSA, vaccine coverage in parts of the UK has declined to the point where R is likely to be near or above 1 in some areas, such as London. This doesn’t mean an outbreak is currently happening, but it does mean there is sufficient susceptibility for cases to potentially grow exponentially if one were to begin.
We can quantify the amount of effort required to stop epidemics using the basic reproduction number (i.e. R if everyone is susceptible). For measles, this value is often cited to be in the 12-18 range (although in reality it is likely to be even more variable than this, depending on population structure and other factors).
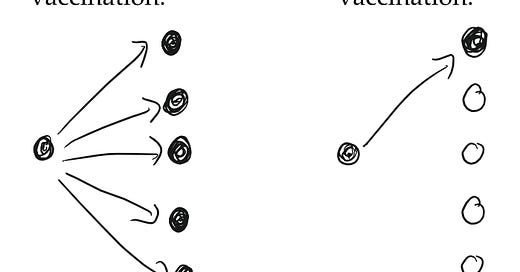
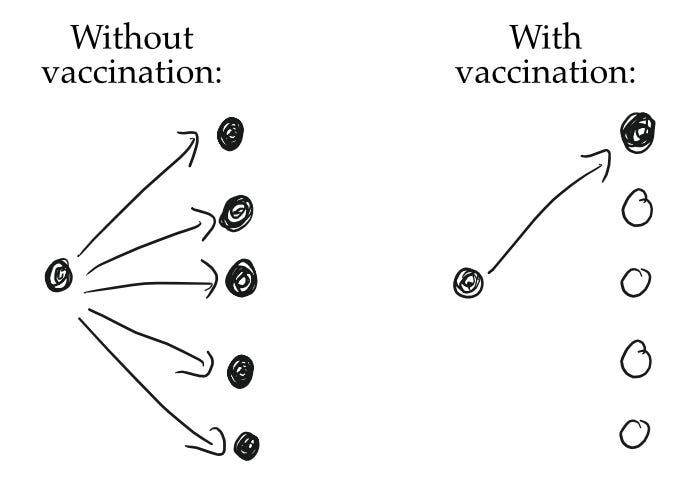
To illustrate the challenge in stopping outbreaks, suppose R was 5 in a fully susceptible population. If a vaccine is 100% effective at stopping infection, we’d therefore need to vaccinate 4 in every 5 people (i.e. about 80% of the population) to bring R from 5 down to 1.
That 80% value – which we call the ‘herd immunity threshold’ for that particular value of R – is the difference between rising and declining transmission. If the basic reproduction number is instead 15, as it can be for measles, the same logic means we’d need to vaccine 14 in every 15 people (i.e. a threshold of 93%). If we’d only vaccinated 90% instead, it would mean 10% are currently susceptible, so our rough estimate of R would be 15 x 0.1 = 1.5.
This is the underlying calculation used in measles risk assessment. However, there are two additional challenges to consider:
Measles vaccines are effective at stopping infection, but not 100% effective (evidence suggests it’s in the high 90s%). This is why the WHO target is 95% coverage with 2 doses of MMR vaccine by age 5.
Not all age groups have the same social contacts, so we need to account for this variation when estimating R. For example, a group of babies who are unvaccinated will not contribute to transmission as much as a group of school children. This can create a delay effect, with a drop in vaccine coverage not immediately showing up as an increase in risk.
Back in 2018, my colleagues and I wrote a comment piece about the concerning number of measles outbreaks in Europe, and the value of prevention through vaccination. ‘Such efforts would come at a fraction of the cost of responding to outbreaks,’ we noted. ‘The Americas have shown that elimination of measles is feasible through a combination of political willpower, targeted interventions, and concerted effort.’
Post-COVID, it looks like the UK – and likely many other countries – will once again need to rise to the challenge.



You mention "population structure". I think this is an area which the field of epidemiology could benefit from better understanding. Not so much for the present question, but for understanding the potential course of future epidemics/pandemics, and identifying the most effective interventions before vaccines become widely available. What groups have the highest density of contacts? How are they interconnected? How does a pathogen spread from one interconnected group to another? Are limited resources better spent protecting vulnerable groups directly, or by preventing it from reaching them in the first place?
Data on population structure seems had to come by—I think because it's hard to acquire. I'd love to hear of research being done in the area.